A few days before this writing, a 32-year-old woman came to
see me for an opinion on stomach pain.
Why would I refuse to see her again?
Abdominal pain is an everyday occurrence for a gastroenterologist. She was accompanied by her mother. I had never met this woman previously.
She had suffered abdominal pains for as long as she could
remember. She recalled frequent visits
with the school nurse when she was a young girl.
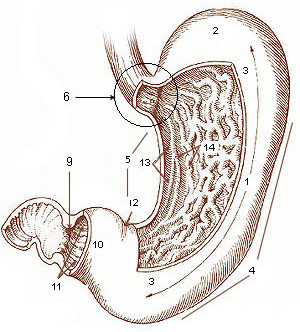
The Stomach - Usually Not the Source of 'Stomach Pain'
She has abdominal distress of varying severity every single
day. Despite this medical history, she was not ill and appeared
well. Why did I refuse to take on her case? She seemed like a very appropriate patient
for my practice. I have expertise in
evaluating and treating abdominal pain. The
patient was pleasant and cooperative. I
believe she would have been comfortable with me as her gastroenterologist.
I learned that the patient lived in another state and was
only in Cleveland to spend the holidays with her family. In fact, she was leaving Ohio the day after
my visit with her. I advised her that
it was not in her medical interest to have a chronic condition managed by a
physician hundreds of miles away.
Sure, I have some folks in the practice who live in other
parts of the country, but I don’t manage their chronic conditions. These people return to Cleveland with some
regularity, and I will do their periodic routine colonoscopies. Conversely, if one of my patients with
active Crohn’s disease is off to Arizona to escape the oppressive Cleveland
winter, I insist that he consult with a gastroenterologist there.
I know we are entering the era of telemedicine. I certainly
do a lot of medicine on the phone every day, and many evenings. But, for many medical issues, there is no
substitute – nor should there be – for a face to face visit with a doctor. Chronic abdominal pain, particularly in a
new patient, can’t be solved in a visit or two. It takes serial office visits over time to
deeply grasp the patient’s symptoms and understand the patient as a person. It needs regular physical examinations,
which is a crucial piece of data for the doctor that can’t yet be acquired
through cyberspace.
Managing chronic disease is a wandering journey for the
patient and physician with unforeseen pitfalls and challenges. Such a patient may awaken one morning with
new symptoms or a flare in his condition and may need to see a doctor on that
very day. Even when the patient’s condition is
relatively stable, there may be phone calls in between visits, or phone calls
to determine the necessity of an office appointment.
So, I didn’t cure her in a half hour, but I did offer her
advice. I recommended that she select a
gastroenterologist where she lived. I
forecasted the conversations that I
anticipated she and the new doctor might have over the ensuing months. She and her mom understood why local medical
care was the proper option for her.
Maybe eventually, my iPhone will have an app that can
palpate an abdomen, discern body language and gauge if a patient ‘looks
sick’. Until then, for most patients I
will rely upon my eyes, my hands and my gut.

Comments
Post a Comment