Here is a potpourri of medical vignettes. All are real life scenarios that I have experienced in my practice. The absurdities of life also permeate the
medical profession. An insider’s view of
medicine, as in any profession or industry, may be less sanitized than its
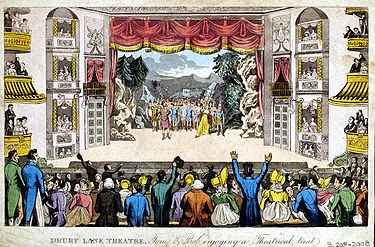
public face. Here are some Scenes from
Scopesville, Ohio.
Act I, Scene I
- Patients are routinely told that they should not eat or drink on the day of their colonoscopy. Recently, a patient decided that these instructions did not prevent him from eating a full breakfast. This is where the phrase, ‘you prepped for nothing’, applies.
- A patient comes to see me on the advice of his primary care physician. He has no idea why he has been sent. Let the sleuthing begin!
- A patient asks for a work excuse for the entire week following his colonoscopy.
- I am asked to fill out disability papers for a patient I saw once a year ago.
- A patient complains to me and my staff about a $20 copay. We have nothing to do with this fee, which is established by the insurance company. He who collects the money must be at fault.
- A patient arrives 45 minutes late and still expects to be seen.
- A doctor arrives 45 minutes late and acts as if he is on time.
- The insurance company denies a patient’s prescription. Of course, these corporate folks deny that they deny anything. They use phrases such as, ‘…the medicine your doctor prescribed is not a covered benefit.’ In other words, they are not technically forbidding the physician from prescribing anything. If it’s the physician’s best medical judgment that his patient needs a $4,000 a month drug, then the insurance company would never block this. They just won’t pay for it.
- A patient is sent to see me who barely speaks English without a translator. This is always fun for me and the staff.
- A patient is transferred to my office from a local nursing home. The documentation explaining the reason for the visit is poor or absent and the patient may be demented or ill to provide meaningful details. This has happened repeatedly. Each time it does, I make a phone call to the nursing home staff and offer a candid and pointed assessment of my view of this inexcusable conduct.
- A patient does not bring in a list of her 11 medications, as every patient is instructed to do.
- A patient asks me, the gastroenterologist, to refill the cardiac medicines.
- A patient wants a referral to a primary care physician. She prefers a female physician. I point out that I am a male.
- A patient asks me how much a colonoscopy costs and is perplexed that I do not know the answer.

Comments
Post a Comment